16 Warning Signs of Lupus to Watch Out For
Friday April 27, 2018 by Marianne Gutierrez 2,707 words
1. Unexplained Fever
Lupus can affect everyone differently and some may have experienced a low grade fever for some time before Lupus is diagnosed. Low grade fevers are generally below 101 degrees F. An unexplained fever does not indicate Lupus as the low-grade fever can be due to any amount of reasons, it is a symptom that combined with other symptoms, or signs, may aid the Doctor to make a diagnosis of Lupus. Doctors look for signs (accepted Lupus signs for example the butterfly rash), symptoms: joint pain, low grade fever, and other common criteria developed by the American College of Rheumatology (ACR) to diagnose lupus.
To help doctors diagnose lupus, this list of 11 common criteria, or measures, was developed by the American College of Rheumatology (ACR). ACR is a professional association of rheumatologists. Rheumatologists are the doctors who specialize in treating diseases of the joints and muscles, like lupus. If you have at least four of the criteria on the list, either at the present time or at some time in the past, there is a strong chance that you have lupus.
Pormezz / shutterstock.com
2. Hair Loss
Unfortunately, in all types of Lupus there will be hair loss, either permanent or for some the hair may grow back. It can affect the hair all over the body not just the head. The hair may become brittle and break easily. Lupus is a disorder of the immune system and it has been found that eating a pure chemical free organic diet, avoiding allergens and only putting chemical free products on the hair, skin and body that the symptoms were reduced.
There are two major forms of alopecia, or hair loss, which can occur in people with lupus. The first form is referred to as “scarring alopecia” which is an area of permanent hair loss usually due to Discoid Lupus Erythematosus (DLE). Discoid lupus generally affects the skin, with most patients never developing the systemic form of lupus … In people with Systemic Lupus Erythematosus (SLE), the most common form of hair loss is “non-scarring alopecia”. This usually consists of thinning of the hair that is not necessarily permanent.
ShotPrime Studio / shutterstock.com
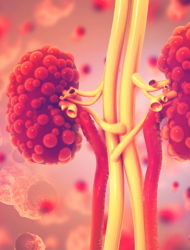
3. Kidney Inflammation
Thirty-five percent of adults in the US have signs of nephritis (inflammation of the kidneys) at the time of a Lupus diagnosis. The treatment is immunosuppressive drugs, corticosteroids, medication to lower blood pressure, a specialist drug to treat SLE and diuretics. The signs of kidney inflammation to look out for are: blood in the urine, foamy urine, pain in the mid-back, swelling of the legs, feet or ankles and sometimes the hands and face.
For this blog, we have enlisted and are honored to have the input of Dr.Donald Thomas, MD, the author of The Lupus Encyclopaedia: A Comprehensive Guide for Patients and Families, for his expert knowledge on lupus. Lupus can present itself with many different symptoms, and these can vary widely in frequency and severity between lupus patients. Lupus nephritis is kidney inflammation caused by systemic lupus erythematosis (SLE) and one of the most serious complications that can result from SLE.
RomarioIen / shutterstock.com
4. Skin Rash
While a rash is a common symptom of Lupus, a rash may not mean you have lupus. However, sometimes the typical rash of lupus can be evident for decades before other symptoms appear and lupus is diagnosed. The rash is not always the butterfly shape either. Therefore this disease can be complicated to diagnose.
More than two thirds of those with SLE develop a rash. However, for every patient with SLE there are two or three where lupus remains confined to the skin.The wide variety of skin manifestations in lupus is illustrated in Table 1, which makes a distinction between lesions which clinically and histologically are characteristic of lupus and other forms of skin involvement that are not so specific for lupus per se, but may be seen in SLE.
Artedmida-psy / shutterstock.com
5. Stiffness & Swelling
Lupus is complicated and can include arthritis in its long list of symptoms, but Lupus is not an arthritic condition. The reason it is important to make this distinction is because the treatments for the two conditions vary considerably. If Lupus was treated as an arthritis, symptoms could be missed and dangerous complications could ensue. Lupus arthritis is caused by inflammation which is seen as stiffness in the joints and swellings.
Lupus is not a form of arthritis, but it does include arthritis as one of the most common symptoms, so it is easy to see why some people think about it that way. It is very important not to make this mistake, because lupus is quite different than any other illness that causes arthritis. It should not be lumped in with these other causes of arthritis, because the causes and the treatments are very different.
fizkes / shutterstock.com
6. Poor Sleep Patterns
Poor sleep patterns seem to arise more after the diagnosis of lupus, although that is not always the case. The condition itself causes physical tiredness due to the wear and tear on the joints, suffering with anemia and the stresses of life combined with living with an illness. Anemia in particular can cause poor sleep patterns.
Putting certain aspects in place may help: going to bed when first tired, reading to switch off the brain so that you can fall asleep, keeping all electronic gadgetry out of the room where you sleep, fresh air, room not too cold. Supplements like omega fish oils and minerals have been shown to calm and aid sleep.
In those with lupus (also known as systemic lupus erythematosus or SLE), the story of fatigue and cognitive dysfunction is what Dr. Melanie Harrison compares to the story of the “chicken and egg.” Each symptom directly impacts the other and can wreak havoc upon the human body by forcing one to endure an ongoing cycle of confusion caused by exhaustion, which is caused by confusion, which is caused by exhaustion, and so on. Such a scenario is hard for individuals to live with and difficult for physicians to diagnose.
Sergey Mironov / shutterstock.com
7. Gastrointestinal Issues
Lupus can affect any part of the body. The cause is due to inflammation which is triggered because of the inefficiency of the body to destroy and get rid of dead cells. The body not only renews and heals cells but has to get rid of cells when they die and has a system in place to action this.
In Lupus this system is impaired. Lupus causes the immune system to create an inflammatory response, which then affects many parts of the body including the gastrointestinal tract (GI). The GI tract runs from the mouth to the anus and the inflammation of Lupus may reduce the secretions that protect the tract that can then cause swallowing problems, acid-reflux, gut pain and gut diseases.
Despite the fact that the knowledge about the etiopathogenesis of SLE has increased in the past few years, there are still unanswered questions. It is well established that a deficiency of the fast and efficient removal of dead cell corpses and debris plays a central role in the course of the disease. Therefore, therapeutic intervention in the vicious cycle of SLE by rescuing the failure of dead cell clearance is a promising approach.
PopTika / shutterstock.com
8. Thyroid Problems
A healthy thyroid needs vitamin A, vitamin B complex, Vitamin C, Vitamin D, Vitamin E, Calcium, Magnesium, Selenium and Zinc.
Thyroid problems for Lupus sufferers arise when the thyroid cannot produce the hormones it needs to maintain the health of the body. Vitamin A is required to convert T4 to T3 a thyroid hormone. If the gut is not able to absorb the nutrients from the diet, then Vitamin A plus a host of other nutrients may be lacking.
Vitamin A is found in animal meat, animal fats, cod liver oil and in liver. The liver can convert betacarotene found in vegetables to Vitamin A, but even in a healthy body that conversion can be difficult. In Lupus sufferers, vitamin A maybe lacking and thyroid problems can result.
An underactive thyroid gland cannot efficiently convert carotene to usable Vitamin A so however many carrots etc. you eat, it won’t help. Vitamin A must also be accompanied by protein to make it available to the body, so if you are on a low protein diet, you may be deficient in this vitamin. If you are low on Vitamin A, your ability to produce TSH is limited. This vitamin is required by the body to convert T4 to T3.
Photographee.eu / shutterstock.com
9. Dry Eyes & Mouth
Sjogren’s disease is a dry mouth. It may also mean dry eyes and vaginal dryness. Due to the inflammatory condition of Lupus, sjogren’s disease may also be diagnosed as nearly all areas of the body are affected by the lupus condition. Therefore, the glands and ducts that supply saliva and lubrication for the body may be malfunctioning.
What can ease the symptoms is to avoid all food intolerance and take mineral, cod liver oil and evening primrose oil supplements. Green lipped muscle supplement may also be beneficial.
Amy Myers MD offers a program to reduce the symptoms of auto-immune disease and has a 5-step program to help reduce the symptoms of Lupus.
Because of the leaky gut autoimmune connection and the huge role your gut health plays in your immune system, repairing your gut is the very first place to begin in reversing any type of autoimmune condition. I use the 4R approach to repairing the gut with my patients, and in all of my books and programs.
Miriam Doerr Martin Frommherz / shutterstock.com
10. Blood In Urine
The role of the kidneys is to get rid of toxins and the kidneys suffer due to the lupus condition. The kidneys with the aid of vitamin D produce an antimicrobial peptide called cathelicidin. If the kidneys are not functioning well this peptide is lacking, further exacerbating the lupus condition and the kidneys.
Lupus nephritis is a condition in which there is blood in the urine making it look pink or light brown. Lupus nephritis causes protein in the urine which makes it look foamy. You may also have swelling in your legs, ankles or around your eyes and experience weight gain and high blood pressure.
Blood and/or foam in the urine will not necessarily mean you have failing kidneys or even that you have Lupus, other tests are required to diagnose this condition. Blood or foam in the urine can be serious and medical advice should be sought immediately.
What are the symptoms of lupus nephritis? Lupus nephritis can cause many signs and symptoms and may be different for everyone. Signs of lupus nephritis include: blood in the urine, protein in the urine, edema, high blood pressure and weight gain.
JPC-PROD / shutterstock.com
11. Seizures
As previously mentioned it is now accepted that Lupus is caused by the body not being able to break down dying cells and get rid of them. When the dying cells are in the brain, this can cause seizures.
Intermediate forms of cell death with both necrotic and apoptotic features have been found after seizures and investigation into the detailed mechanisms of the different forms of cell degeneration is needed before attempts to specific prevention can be made.
The seizures may also be due to interventions by the GP, by medication or metabolism.
Seizures associated with systemic lupus erythematosus (SLE) occur in 9 to 58% of patients in reported series, often early in the disease course. Approximately half of seizures reported in SLE patients are associated with infection and with metabolic or iatrogenic complications. However, in clinical practice, this number might be much larger, as relatively few prospective studies are available. The seizure type in nearly 75% of SLE patients is generalized tonic-clonic.
Rainer Fuhrmann / shutterstock.com
12. Depression
Depression can be divided into two types, temporary feelings of negativity and clinical depression. With Lupus, temporary feelings of negativity occur as one gets used to a different lifestyle, but with help the negative feelings may dissipate. Clinical depression is when the sufferer has been depressed, irritable, decreased energy, lack of interest in hobbies and activities for more than a few weeks.
In Lupus sufferers, clinical depression is difficult to realize because the symptoms tie in with the symptoms of the disease.
Life with lupus can be challenging. With symptoms that come and go, disease flares and remissions, and the uncertainty of what each day will bring, it’s normal to experience feelings of unhappiness, frustration, anger, or sadness. It’s also normal to grieve for the loss of the life you had before lupus.
aslysun / shutterstock.com
13. Frequent Infections
Lupus sufferers do have a lowered white blood cell count, but it is thought not to be enough to lead to an infection. However, because of their lowered immune function, if an infection is present, it may trigger the Lupus symptoms, a flare up and worsening symptoms.
Infection is known as one of the common trigger factors for SLE; there are a number of reports on infectious agents that provoke autoimmune response. Several viruses, bacteria, and protozoa were revealed to cause immune dysfunction by molecular mimicry, epitope spreading, and bystander activation. In contrast, certain pathogens were revealed to protect from immune dysregulation. Infection can be threatening to patients with SLE who have a compromised immune system.
nobeastsofierce / shutterstock.com
14. Bruising & Bleeding
This is caused by thrombocytopenia which is a deficiency of platelets in the blood. It causes easy bruising, bleeding into the tissues and slow blood clotting. However, not all patients diagnosed with Lupus suffer with thrombocytopenia.
Thrombocytopenia can be a symptom of other diseases and if you see severe bruising on your body for no particular reason you must see your Medical Practitioner immediately.
In conclusion, the severity of thrombocytopenia in SLE patients can be a useful independent prognostic factor to predict survival. Moreover, response to treatment of thrombocytopenia is also important because failure to achieve complete remission of thrombocytopenia has a close association with mortality. The severity of thrombocytopenia and the response to treatment should be closely monitored to predict the prognosis in SLE patients.
andriano.cz / shutterstock.com
15. Chest Pain
Inflammation and the peculiarities of the immune system cause the arteries in the heart to harden (atherosclerosis) and someone with Lupus is more likely to suffer with heart disease. Heart disease can cause chest pain. The good news is that researchers are making great inroads into the cause of Lupus and what can be done to treat it.
The cardiovascular system is a main target of lupus. It can directly weaken the heart by causing inflammation of the muscle itself (myocarditis) or its inner lining (endocarditis). But the most common heart involvement in people with lupus is inflammation in the sac around the heart (pericarditis), which causes shortness of breath and sharp chest pain. These complications are typically treated with powerful anti-inflammatory and immune system suppressants such as prednisone, a corticosteroid.
CHAjAMP / shutterstock.com
16. Mouth & Nose Ulcers
Mucous membranes lining the mouth, respiratory tract and inside the nose secrete mucus and saliva which lubricates and protects. More mucus is secreted when the immune system senses a pathogen. In a lupus flare up, the secretion of mucus and saliva is affected, causing lesions inside the mouth and nose forming ulcers. This may be due to Sjogren’s syndrome where white blood cells target healthy cells in the moisture producing glands.
About 25% of people with lupus experience lesions that affect the mouth, nose, and sometimes even the eyes. These lesions may feel like small ulcers or “canker sores.” Such sores are not dangerous but can be uncomfortable if not treated. If you experience these types of lesions, your doctor may give you special mouthwash or Kenalog in Orabase (triamcinolone dental paste) to help expedite the healing process.
9nong / shutterstock.com

16 Warning Signs of Lupus to Watch Out For
1. Unexplained Fever Lupus can affect everyone differently and some may have …


21 Features of Kidney Disease
1. Dizziness Kidney Disease is when the kidneys are not filtering blood …

Top 10 Foods to Nourish Your Thyroid
Did you know that the food you eat can affect your thyroid health? Some foods …


12 Facts About Your Borderline Personality …
1. It's Finally Classified As a Mental Illness Borderline Personality Disorder, …


12 Common Factors That Trigger Rosacea …
1. Makeup Some products used on the face and body or in the mouth ie: make-up, …


22 Common Symptoms of Type II Diabetes
1. Mood Changes Mood change is sometimes one of the first symptoms to suggest …
